Preimplantation genetic diagnosis (PGD) is a reproductive technology used with an IVF cycle to increase the potential for a successful pregnancy and delivery. It is a genetic test on cells removed from embryos, to help select the best embryo(s) for pregnancy or to be free of a genetic disease.
PGD may be considered in all IVF cycles; however, those who might benefit most from this test are couples at increased risk for chromosome abnormalities or specific genetic diseases. This includes women who have had several miscarriages, or who have had a prior pregnancy with a chromosome abnormality. Women over 38 years of age and men with some types of sperm abnormalities may also produce embryos with higher rates of chromosome abnormalities. In addition, if a person carries a rearrangement of the chromosomes, PGD can identify which embryos have a normal amount of chromosomal material. When there is a 25% or 50% chance to have a child affected with a specific genetic disease, PGD can be designed to identify which embryos are affected, unaffected, or a carrier (if applicable) for that disease. Then, only embryos without the disease are transferred to the uterus to attempt pregnancy.
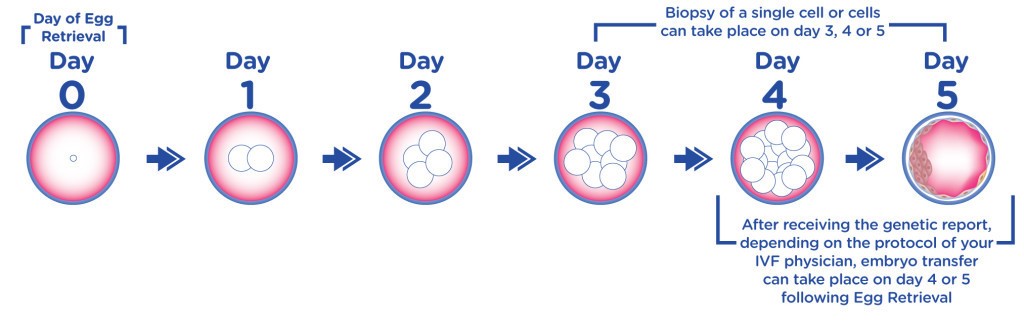
After embryos are created in the laboratory, they are grown for five to six days. On day 3 or in day 5, the biopsy for PGD is done on all appropriately developing embryos.
In the case of PGD on day 3, biopsy involves removing one cell from the embryo; this cell will be genetically tested and will carry the genetic make up of the embryo. Our team will discuss PGD test results with the woman/couple, and a fresh embryo transfer on day 5 will be planned. Only the genetically normal embryos will be transferred.
In the case of PGD on day 5, biopsy involves removing a one few cells from the trophectoderm, or the layer of cells that is ‘hatching out’ of the embryo at this stage of development. The embryos are stored while genetic material inside the removed cells is tested for abnormalities. Our team will discuss PGD test results with the woman/couple, and a frozen embryo transfer (FET) cycle is planned for use of the embryo(s). Only the genetically normal embryos will be transferred.
Yes. In embryos where chromosomal microarray testing is performed, one can expect fewer pregnancies with chromosomal disorders since most chromosomal disorders are identified prior to transfer of the embryos to the uterus. Removal of a few of the cells of the early embryo does not alter the ability of that embryo to develop into a complete, normal pregnancy.
Preimplantation genetic diagnosis
Only the genetically and morphologicaly normal embryos will be transferred. While embryo morphology is helpful in selecting the best embryos for transfer, it is known that many embryos with significant chromosome abnormalities have normal morphology. Therefore, PGD results help to better identify the best embryos to transfer to the uterus. The combination of normal genetic testing with normal physical appearance indicates the highest chance of becoming a healthy pregnancy. All decisions regarding which embryo(s) to transfer to the uterus and how to use the remaining embryos are made together between the couple and their medical team.
