In Vitro Fertilisation (IVF) was developed in the 1970s as a treatment for infertility due to the tubal factor, but it has proven an efficient treatment for patients suffering from endometriosis, ovulatory disfunction, infertility caused by poor sperm quality, genetic conditions and infertility of unknown origin.
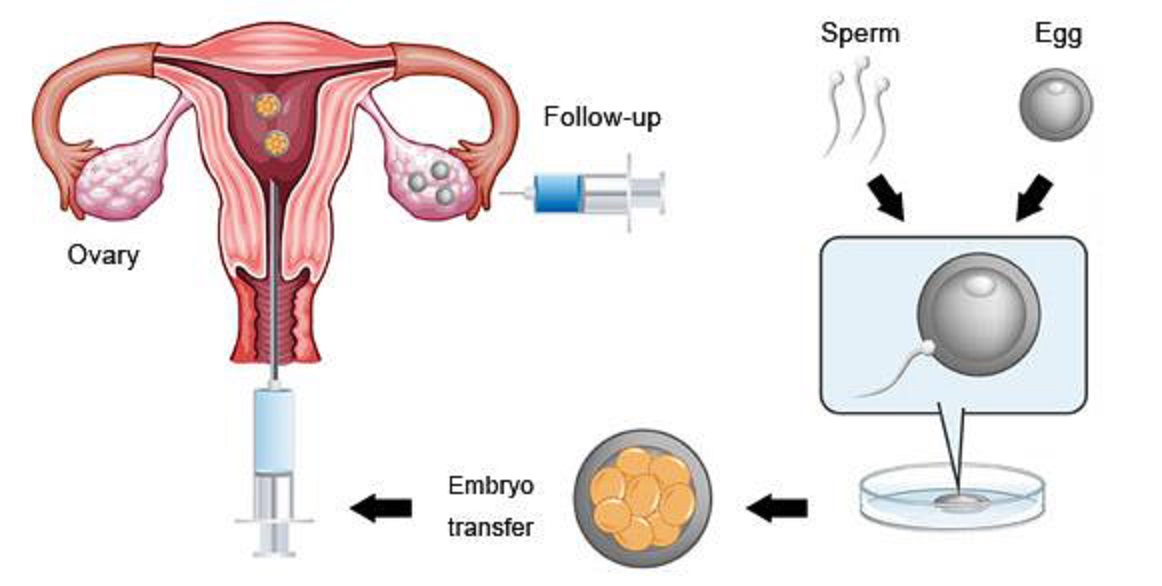
Fig. IVF procedure made easy
In-Vitro Fertilization (IVF) is a technology that introduces the female egg (oocyte) and male sperm together in a specialized culture medium (outside of female body hence the term in vitro) where the chances of successful fertilization are greatly enhanced. The embryos are observed and grown in our IVF laboratory, where they are graded for quality and reintroduced to the recipient's uterus at a multicell embryo stage or later at the blastocyst embryo stage. All procedures required during an IVF cycle, including ovarian stimulation and monitoring, egg retrieval, and embryo transfer, are performed on-site in our state-of-the-art facilities.
Fertilisation of the egg by the sperm involves a complex sequence of events, initially controlled by the sperm.
Classical IVF and intra-cytoplasmic sperm injection (ICSI) are the two most popular assisted reproductive technologies used for successful fertilisation. The only difference between the two is the way the egg is fertilised. IVF allows the sperm to penetrate the egg of its own accord whereas ICSI directly inserts the sperm into the egg
ICSI (Intracytoplasmic Sperm Injection) bypasses the work the sperm otherwise has to do during fertilisation. The eggs are placed in a shallow dish in microdroplets of culture medium under oil, arranged around a central drop containing sperm. The embryologist captures sperm one at a time using fine glass needles attached to manipulators mounted on a microscope. The embryologist then moves to a drop containing an egg, holds the egg with another fine pipette, and injects the sperm deep into the egg.
As part of the ICSI procedure, the embryologist breaks the egg’s membrane to trick the egg into thinking it has been fertilised in the normal way. The embryologist also breaks the sperm’s tail before injection to allow chemicals to escape from the sperm into the egg, and so signal that the sperm is present and ready to be ‘unpackaged’.
ICSI can work because in most men the genetic make-up of sperm is normal even though the sperm might be abnormally shaped, unable to move very well, or unable to undertake the steps of normal fertilisation.
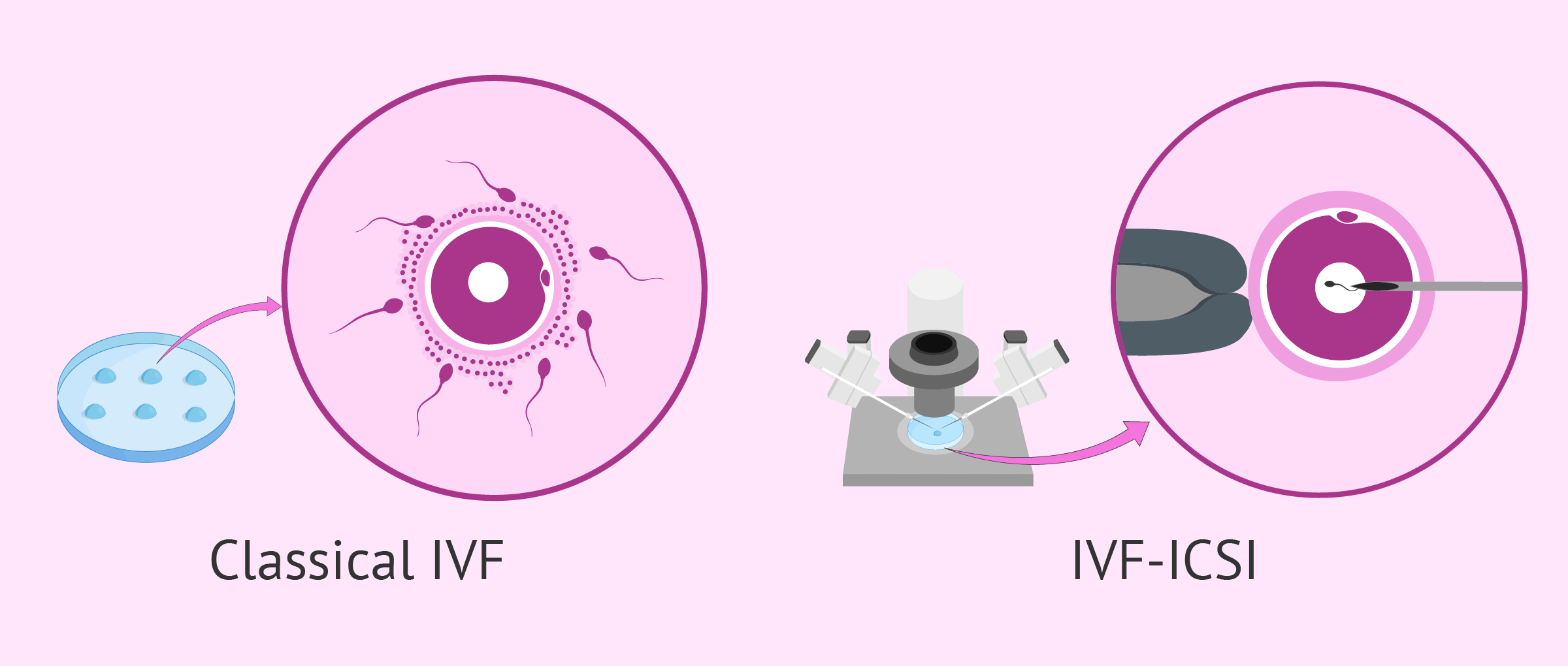
Conventional (classical) IVF vs ICSI
IVF was originally developed for women with blocked fallopian tubes or missing tubes and is still used to treat those conditions. It is also used when infertility cannot be explained and with the following ovulatory or structural causes:
- problems with ovulation
- endometriosis
- fibroids
- polycystic ovarian syndrome
- cervical problems
ICSI is usually offered to couples who have had poor or no fertilisation during standard IVF but is mainly used to overcome male infertility. It was first used in 1992 and offers an alternative to donor sperm for those who have severe male infertility, which includes:
- poor sperm morphology (abnormally shaped sperm)
- poor sperm motility (slowly moving sperm)
- a low sperm count
- an obstruction that prevents sperm release (such as vasectomy)
- antisperm antibodies (antibodies produced by the man’s body, which may inhibit sperm function)
- poor oocyte morphology
